PrEP in All Shapes and Sizes at AIDS 2024

The AIDS 2024 conference in Munich showcased major advances across an array of new HIV prevention options. While the results of the Phase III lenacapavir for PrEP trial, PURPOSE 1, took centre stage, more data on cabotegravir for PrEP expanded who can take it, and important conversations were underway on the Dual Prevention Pill. The importance of choice, acknowledging that no one HIV prevention product will meet everyone’s needs, also permeated the conference.
Zero Infections
One of the most significant advances in the history of HIV prevention, the efficacy of lenacapavir as PrEP, was presented at the Co-Chair’s Choice session. The findings, zero infections and 100% efficacy among the trial participants in the PURPOSE 1 trial, brought a standing ovation.
Presented by Linda-Gail Bekker of the Desmond Tutu Health Foundation, and published in the New England Journal of Medicine, PURPOSE I enrolled 5,300+ cisgender adolescent girls and young women (ages 16-26) in South Africa and Uganda. PURPOSE 1 also evaluated daily oral emtricitabine/tenofovir alafenamide (F/TAF) for PrEP, which was shown to be safe. Overall adherence in the F/TAF arm of the trial was low, and the intervention did not show overall efficacy. But, among those trial participants with medium to high adherence (2-4 doses per week), data showed a significantly lower chance of HIV infection compared to participants with low adherence.
For more on PURPOSE 1 and the rest of the PURPOSE program evaluating lenacapavir across diverse populations, see AVAC’s primer for advocates, The Lens on LEN.

CAB for PrEP for PLP
New findings from the injectable cabotegravir for PrEP open label extensions could increase access.
Pregnancy and the post-partum period are times of heightened risk of HIV transmission. Findings from the HPTN 084 open label extension (OLE) showing that CAB is safe to use during pregnancy come as welcome news, providing pregnant and lactating people (PLP) with an additional safe HIV prevention option. Now it’s up to government regulators to ensure that local CAB for PrEP guidelines reflect these findings and include indications for use by PLP.
Analysis from the other CAB for PrEP OLE, HPTN 083, found that RNA testing is not recommended for CAB continuation. This is in line with long-standing WHO guidance that rapid diagnostic testing (RDT) is sufficient for use with CAB for PrEP initiation and continuation. RNA testing is more expensive than RDT and requires a lab, making it much less widely available in lower resource settings, so requiring it for use with CAB for PrEP would severely limit access to a highly effective method of HIV prevention. This finding should provide additional reassurance to implementers and national ministries of health that RDTs are the appropriate method of HIV testing for use with CAB for PrEP.
As one of the first countries to integrate CAB for PrEP into their national PrEP programme, Zambia has an important role to play in generating early insights. Initial reports from Zambia’s experience were encouraging, with CAB for PrEP continuation rates at similar high levels to oral PrEP delivered at the same sites, leveraging best practices established from oral PrEP provision. It will be important for Zambia and other early adopters of CAB for PrEP to continue this monitoring and sharing what they learn for the success of future CAB for PrEP programmes all over the world.
All these early CAB for PrEP insights and more can be found in the new CAB for PrEP evidence gap tracker– check back regularly for real-time updates.
From Condoms to the DPP: What’s up with MPTs?
The Dual Prevention Pill (DPP) combines PrEP with a contraceptive, and is working its way toward regulatory submission. Once approved, it will be the first multipurpose prevention technology (MPT) to enter the market since condoms. In a workshop on the DPP, Two for the price of one: Simplifying access to HIV prevention and contraception with multipurpose prevention technologies, attendees brainstormed how to address real-world dilemmas that may come with rolling out the DPP. These dilemmas include how to train HIV and family planning providers to deliver the DPP and how governments and donors will balance the delivery of all proven methods for HIV prevention, including CAB for PrEP and the ring. Proposed solutions touched on the importance of stakeholder engagement, models for demand creation and more. To learn more about the DPP and the full pipeline of MPTs, see AVAC’s Advocates’ Guide to MPTs.

PrEP Choice: Ensuring a range of PrEP products are available
Several sessions at AIDS 2024 focussed on the importance of choice now that PrEP comes in many forms— rings, pills and injections, with hopefully more on the way.
First was the preconference session, Welcome to the Era of PrEP Choice, organized by the Gates Foundation, Unitaid, USAID, and the World Health Organization, which reinforced that everyone has a role to play in expanding access to real choices for everyone who needs HIV prevention. Putting in place the right programs, policies and investment to deliver choices at scale depends on a commitment to integrated and community-led approaches.
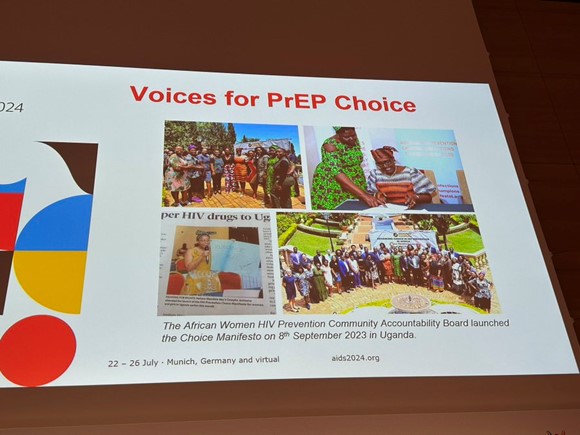
Meanwhile, the African Women’s Prevention Community Accountability Board (AWPCAB) continued to raise their voices and call on the international community to prioritize expanded access to existing products, such as the dapivirine vaginal ring (DVR) and injectable cabotegravir, and to developing new methods to ensure a range of prevention options for women and girls. Winnie Byanyima of UNAIDS reinforced her commitment to the Choice Manifesto, a declaration put forward by AWPCAB, calling for sustained political and financial support for more choice in HIV prevention.
Later in the week, during the satellite HIV Prevention in the Time of Choice, Michelle Rodolph from WHO confirmed they are “supporting PrEP options, also PrEP choice, prevention choice, and that includes the DVR, and we’ll continue to include the ring in all of our guidance moving forward.” Next steps for making choice a reality included curricula for training healthcare workers; more PrEP options for pregnant and lactating people; reducing costs through local manufacturing and technology transfers; and of course, community engagement.
Finally, in the plenary HIV Prevention Strategies, Jhpiego’s Elizabeth Irungu decried the historical delays in the rollout of oral PrEP and called on all stakeholders to break the 12-year cycle of squandering opportunities in prevention.